The Science & Theory of Therapeutic Spinning in Vestibular Rehabilitation
An Introduction for the Curious Therapist
Welcome. The article you are about to read delves deep into the science behind one of vestibular therapy's most potent tools: therapeutic spinning. Be prepared; some of these concepts are complex and may feel a bit overwhelming at first, especially if you are new to this level of neurophysiology. That's okay. For any therapist who treats dizziness, understanding the principles of rotation is not just an academic exercise—it is fundamental to becoming an expert in the field. I encourage you to embrace the learning process. Revisit sections as needed. A solid grasp of this material will transform your approach, moving you from simply following protocols to truly understanding and manipulating the neurological systems you aim to heal.
A History of Spin: From Elite Performance to Clinical Prescription
Long before physical therapists began using controlled rotation in the clinic, the world's most demanding professions were already harnessing the power of spin. Figure skaters, gymnasts, fighter pilots, and astronauts have all utilized spinning not just as part of their job, but as a critical tool to force their brains to adapt to extraordinary environments. Understanding why they do it reveals the fundamental principles we now apply to our patients.
The Performer: Skaters & Gymnasts
When you watch a figure skater perform a high-velocity spin or a gymnast execute a multi-axis tumble, you are witnessing an extreme example of neurological mastery. For them, the goal of repeated spinning is to suppress VOR. Through thousands of hours of practice, their brains learn to actively inhibit or suppress the vestibulo-ocular reflex. They couple this neurological adaptation with behavioral strategies like 'spotting', where they fixate their gaze on a single point to minimize retinal slip and provide a stable visual anchor in a swirling vestibular world.
The Pilot: Overcoming Spatial Disorientation
For a fighter pilot, vertigo is a fatal risk. They are systematically exposed to disorientation in training devices to learn two things: to recognize the feeling of sensory illusion, and to follow the cardinal rule of aviation: 'trust your instruments, not your instincts'. The training is designed to prove that their innate sense of balance is fallible and that survival depends on ignoring it.
The Astronaut: Rewriting the Rules of Balance
In the microgravity of space, the vestibular system is thrown into chaos. Astronauts undergo pre-flight adaptation training, where they are spun in rotating chairs to kickstart the process of 'sensory re-weighting'. The goal is to teach the central nervous system to rapidly down-regulate its reliance on now-useless gravity signals and place more trust in visual cues.
The lesson from these fields is clear: the human brain, when subjected to a robust and consistent rotational stimulus, will do whatever it must to adapt. If spinning can forge the nervous systems of elite performers, we can harness those same fundamental principles to heal our patients.
https://www.britannica.com/science/ear/The-physiology-of-balance-vestibular-function
The Inner World: A Deeper Dive into the Dance 🧠
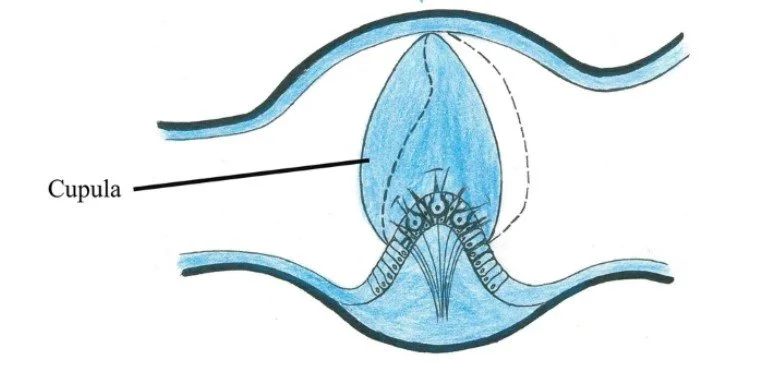
Your sense of motion comes from the semicircular canals. At rest, vestibular nerves from both ears send a balanced, 'tonic firing rate' to the brain. When your head turns, the fluid (endolymph) lags, causing a 'cupular deflection'. A key principle here is that excitation (an increase in firing rate) is a more potent signal than inhibition (a decrease in firing rate), which is limited by the 'inhibitory cut-off'. In a unilateral vestibular hypofunction (UVH), this system is broken. The tonic rate is imbalanced, creating a constant error signal. Our job is to use targeted motion to convince the brain to fix this error.
https://slideplayer.com/slide/14649344/
Key Concept - Inhibitory Cut-Off: A vestibular nerve's firing rate cannot drop below zero spikes per second. This physiological floor means that while a nerve can increase its firing rate significantly (excitation), it has a hard limit on how much it can decrease its firing rate (inhibition). This asymmetry is a critical factor in vestibular disorders.
The Critical Nuance: Cupular Dynamics and the Two Forms of Adaptation
The effectiveness of spinning as a treatment hinges on understanding exactly how the cupula behaves over time and why the direction of spin is the most crucial decision a therapist can make. Let’s discuss these in the next section.
The Physics of Cupular Deflection and Rebound
DOIhttps://doi.org/10.1038/s41598-021-87730-w
When a constant velocity spin begins, the cupula deflects instantly due to the lagging endolymph. However, the cupula is an elastic structure. It wants to return to its neutral position. Due to these elastic restoring forces, the cupula will slowly return to its primary, undeflected position over the course of approximately 7 to 11 seconds, even if the spin continues at a constant speed. This is a critical point: the mechanical sensor itself effectively 'resets' mid-spin. This is why the brain's 'velocity storage mechanism' is so important.
Key Concept - The Velocity Storage Mechanism: Imagine a small internal reservoir in your brainstem that holds onto the feeling of rotation. Even after the cupula has returned to its neutral position during a constant spin, this mechanism continues to fire, telling your brain you are still turning. It essentially prolongs the neural signal of rotation beyond the physical stimulus. This is crucial for our perception of smooth, continuous turns.
When the spin suddenly stops, the endolymph's momentum creates a decisive 'rebounding cupular deflection' in the opposite direction. Now, the cupula is signaling a decisive turn in one direction, while the velocity storage mechanism is often still active from the original direction of spin. This mismatch is the massive sensory conflict we use for therapy.
The Strategy: Two Forms of Adaptation Stimulus
The direction we spin is a deliberate choice to produce a specific neurological effect, leveraging two different types of adaptation stimuli.
Short Spins Toward the AFFECTED (Weak) Side: The Direct Adaptation Stimulus. Short spins are a potent tool for adaptation. By spinning toward the weak ear, we create a direct and consequential excitatory cupular deflection on that side. This is a clean, predictable, real-time error signal presented to the brain. The brain's attempt to correct the VOR during this brief, intense stimulus drives a specific form of adaptation. The goal is twofold: first, to stimulate and up-regulate the weak side with a direct excitatory current, and second, to drive adaptation by forcing the brain to improve its response to that specific, brief movement.
Long Spins Toward the UNAFFECTED (Strong) Side: The Rebound Adaptation Stimulus. The long spin uses a different mechanism. During the constant-velocity spin toward the strong side, the system effectively neutralizes as the cupula returns to its baseline position. The actual therapeutic event is referred to as the 'post-rotational stimulus'. When you stop, the rebound deflection creates a powerful and prolonged inhibitory signal on the strong side. This results in a very robust post-rotary nystagmus beating toward the strong side. The patient's brain is then forced to contend with this massive, sustained error signal after the motion has ceased. Its effort to suppress this intense nystagmus is what drives a profound central adaptation, forcing a recalibration of the faulty 'velocity storage mechanism'. We are using the strong side to create a powerful rebound event that trains the brain's central processing and error-correction circuits.
Conclusion
Understanding the science behind therapeutic spinning transforms it from a simple exercise into a precise neurological instrument. We've seen how its principles are used to forge the nervous systems of elite performers and how we can apply that same power in the clinic. The dance between the cupula and the endolymph, the critical 7-11 second reset, and the strategic use of a 'direct' versus a 'rebound' adaptation stimulus are not just academic details—they are the very foundation of your clinical decision-making.
With this deep understanding of the 'why', we can now confidently transition from theory to practice. The following section, Part 2, will provide the clinical framework to translate this knowledge into safe, targeted, and profoundly effective treatment.